- Eruption of primary teeth
- Problems during the eruption of deciduous teeth
- Signs and symptoms of teething
How primary teeth come through

Despite many theories, no one really understands or knows the exact mechanism for tooth eruption of primary and adult teeth. The periodontal ligament, which is the ligament that joins the tooth to the bone, is thought to be responsible for pushing the tooth from the jawbone, to the mouth.
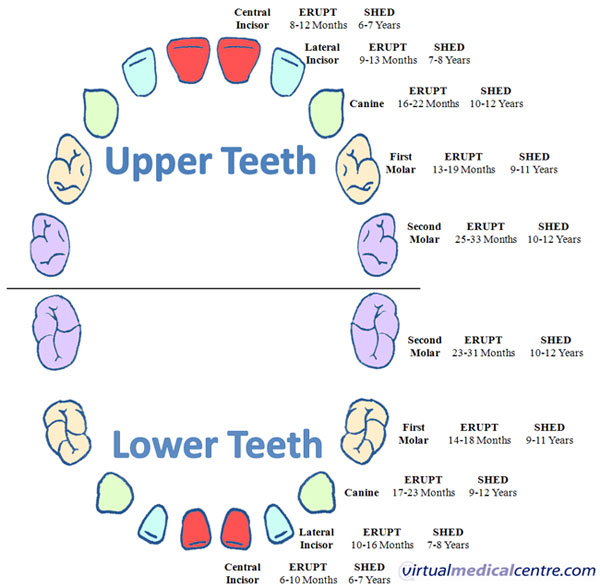
When the primary teeth come through
The time that teeth come through (erupt) can vary, but as a general rule, the tooth will usually come through within 3-6 months of the below timeframes:
Problems during the eruption of deciduous teeth
Delay in eruption of primary teeth has been noted in hypopituitarism, hypothyroidism, Down’s syndrome, cleidocranial dysostosis, Gardener’s syndrome, and cerebral palsy, to name a few. Diseases that affect the endocrine glands and are of genetic cause more commonly result in delayed eruption.
Eruption cysts are a type of fluid filled sac that forms on the top of a tooth that is coming through. The cysts are often blue, raised, able to be compressed and oval shaped. It may form during the period of eruption of the primary or adult teeth. More often than not, eruption cysts go away as the tooth comes through.
In the past, eruption cysts were often misdiagnosed as ‘dentigerous cysts,’ which is another type of cyst that must be managed differently as it does not resolve as the tooth comes through.
The type of treatment provided for eruption cysts ranges from no treatment to extraction of the tooth and removal of the cyst. The best form of treatment is to leave it alone as eruption cysts are often of no consequence and resolve when the tooth comes through.
If there is no improvement after the tooth comes through, then it is possible that the lesion is not an eruption cyst, and another form of treatment should be considered.
Natal teeth (those which come through around the time of birth) usually occur in around 1 in 2,000 to 1 in 3,500 births. Most of the natal and neonatal teeth (those which are present at birth) are normal teeth that just come through more quickly than usual. There is a chance that the natal or neonatal tooth is actually an extra tooth (supernumerary tooth). This is usually the cause in around 1-10%.
If the natal or neonatal tooth is an extra tooth, then it is usually removed by the dentist. Extraction is also best for very mobile teeth due to the risk of the tooth falling out and subsequent swallowing or inhalation.
Riga-Fedes syndrome, occurs in approximately 6-10% of cases of neonatal or natal teeth. It is, essentially, the ulceration and infant discomfort that occur when primary teeth come through. As there are difficulties with having teeth at this young age, Riga-Fedes syndrome can be managed by:
- Extraction of the offending tooth;
- Grinding or discing to remove the roughness, bumps and any sharp edges associated with any given tooth;
- Coverage of the tooth/teeth with a filling material (composite resin) to provide a smooth rounded surface; and/or
- Stomahesive wafers to cover the teeth and provide a smooth surface for the tongue to pass over during suckling.
Get on top of your dental health
Find and instantly book affordable dentists within Australia
Signs and symptoms of teething

By 1839, 5,016 deaths in England and Wales were supposedly attributed to teething. Teething was used to account for the following infant deaths in London:
- 4.8% of all deaths under the age of 1 year;
- 7.3% of deaths between the ages of 1 and 3; and
- 12% of all deaths under 4 years.
The belief in lancing the gums was widely and firmly held by both the medical profession and the public, something that is now considered obsolete.
As recently as 1979, parents and physicians were identifying teething as a cause of presenting symptoms in children admitted to the hospital. The problems ranged from upper respiratory infection to bacterial meningitis, and it was found that most of these cases were easily attributed to another cause.
Good evidence now exists that teething is associated with, at most, minor and relatively infrequent symptoms. Most medical professionals now agree that teething does not cause life-threatening illness.
Teething appears to be linked with:
- Daytime restlessness;
- Thumb-sucking;
- Gum-rubbing;
- Drooling; and
- Loss of appetite.
A slight fever, facial rash, sleep disturbance, and ear rubbing may all be associated with teething, however it must be stressed the link is likely to be small, if at all there is one.
Biting, drooling, gum-rubbing, irritability, and sucking are all common symptoms 3 or 4 days before and after primary teeth come through, whereas decreased appetite for solids, wakefulness, ear-rubbing, facial rash, and slight fever all appear to be possible symptoms 1 or 2 days before and after teeth come through.
It is thought that teething is the scapegoat for many other events occurring between about 6 and 24 months of age, after a relatively trouble-free first 6 months of life. These may include the sudden rise in respiratory, middle ear, and diarrhoeal infections at this age as well as specific infections such as herpes simplex virus (predominantly type 1).
Severe symptoms such as fever, diarrhoea, strong urine, and susceptibility to infections do not appear to be associated with teething; it is safe to say that serious and life-threatening problems are not linked to teething.
Treatment of teething
Home remedies and conservative treatment

Other home remedies include chewing breadsticks and oven-hardened bread, frozen breads, a variety of fresh and frozen fruit and vegetables, and providing infants with a pacifier for temporary pain relief.
Several of these remedies involve applying pressure to the painful area. You can also apply mild pressure with a clean finger (possibly with wet gauze) or a cold spoon. Excess saliva can run onto the infant’s skin. It should be wiped away regularly or a facial rash may develop.
Most parents prefer to avoid using drugs and medications during teething; however, a wide range of effective local (applied to the tooth) and systemic (affect the body systems) treatments are available when simple remedies do not provide relief. These remedies at best only last a few minutes, so their effectiveness is questionable, nonetheless they are commonly used.
Sugar-free paracetamol reduces pain and fever, and is the most common form of drug-based treatment.
Lignocaine hydrochloride is a local anaesthetic that is rapidly absorbed in the mouth, giving quick relief from pain, although temporarily. It is used commonly for dental procedures, and it should be applied cautiously in infants to prevent an overdose.
Choline salicylate is the active ingredient of several minor pain medications commercially sold for teething issues, and is similar to aspirin. Although Reye syndrome, (a disorder of the liver and nervous system) is related with the use of aspirin in children, it appears choline salicylate does not present a problem. However, many paediatricians and pharmacists now tell people to avoid choline salicylate preparations in teething for possible safety reasons.
Long-held cultural beliefs about teething should be put to rest, and it is time to acknowledge that there is good evidence that teeth coming through are not associated with significant symptoms. Those children with symptoms that were historically thought to be related to teething e.g. diarrhoea, herpes simplex virus, and other severe infections should not be subjected to the treatment modalities of teething, and professional help should be sought instead.
Adding sugar, honey or jam to feeding bottles, or dipping a pacifier in honey or jam has absolutely no pain relieving effect, and will cause tooth decay. Repeated application of alcohol to the mucous membrane of an infant is ineffective and due to an infant’s small body weight, may lead to severe problems.
Key points
The time when a baby’s first few teeth begin to erupt is called teething.
- Most children have all 20 of their primary teeth by their 3rd birthday.
- Often the gums around the new teeth may cause:
- Swelling and tenderness;
- Restlessness;
- Irritability;
- Crying;
- Slight temperature;
- Excessive drooling, leading to a possible rash;
- Disruption of eating and sleeping habits; and/or
- A desire to bite something hard or rub on the gums.
- Teething does not cause serious health problems such as high fever, vomiting, convulsions and diarrhoea.
- Manage teething by:
- Gently rubbing or massaging the gums with a finger to help the baby’s discomfort;
- Natural means such as ice cubes wrapped in cloth or cold food items; and/or
- Teething rings.
- Try to keep the child’s face dry. Wipe it often with a cloth to remove the drool to avoid a rash forming on the baby’s face.
- Pain relievers and medications you rub on the gums are not highly effective over long periods of time, since they wash out of the baby’s mouth within minutes.
- Do not use any medications that contain alcohol, as they can be toxic. Avoid sugar, honey and jam on pacifiers too as it will lead to tooth decay.
- If symptoms continue to worsen, then it may be recommended to use medications such as paracetamol.
Kindly written by Dr Akhil Chandra BDSc. (Hons UWA)
Dentist, Whitfords Dental Centre and Editorial Advisory Board Member of the Virtual Dental Centre
More information
 |
For more information on dental health and hygiene in children aged 0 to 5 years, see Dental Health in Kids. |
References
- Ashley MP. It’s only teething…a report of the myths and modern approaches to teething. Br Dent J. 2001; 191(1): 4-8.
- For the dental patient. Tooth eruption: The primary teeth. J Am Dent Assoc. 2005; 136(11): 1619.
- Proffit W. Contemporary Orthodontics. 3rd ed. St Louis: Mosby, Inc; 2000.
- Marks SC Jr, Gorski JP, Wise GE. The mechanisms and mediators of tooth eruption-models for developmental biologists. Int J Dev Biol. 1995; 39(1): 223-30.
- Marks SC Jr, Schroeder HE. Tooth eruption: Theories and facts. Anat Rec. 1996; 245(2): 374-93.
- Arvystas MG. Early eruption of deciduous and permanent teeth: A case report. Am J Orthod. 1974; 66(2): 189-97.
- Lammert M, Friedrich RE, Friedman JM, Mautner VF, Tucker T. Early primary tooth eruption in neurofibromatosis 1 individuals. Eur J Oral Sci. 2007; 115(5): 425-6.
- Boyden TW, Hanson F. Hypopituitarism, delayed growth, and an empty sella turcica. Am J Med Sci. 1981; 282(2): 75-9.
- Mg’ang’a PM, Chindia ML. Dental and skeletal changes in juvenile hypothyroidism following treatment: Case report. Odontostomatol Trop. 1990; 13(1): 25-7.
- Ondarza A, Jara L, Munoz P, Blanco R. Sequence of eruption of deciduous dentition in a Chilean sample with Down’s syndrome. Arch Oral Biol. 1997; 42(5): 401-6.
- Smylski PT, Woodside DG, Harnett BE. Surgical and orthodontic treatment of cleidocranial dysostosis. Int J Oral Surg. 1974; 3(6): 380-5.
- Buch B, Noffke C, de Kock S. Gardner’s syndrome – the importance of early diagnosis: A case report and a review. SADJ. 2001; 56(5): 242-5.
- Pope JE, Curzon ME. The dental status of cerebral palsied children. Pediatr Dent. 1991; 13(3): 156-62.
- Suri L, Gagari E, Vastardis H. Delayed tooth eruption: pathogenesis, diagnosis, and treatment. A literature review. Am J Orthod Dentofacial Orthop. 2004; 126(4): 432-45.
- Woldenberg Y, Goldstein J, Bodner L. Eruption cyst in the adult-a case report. Int J Oral Maxillofac Surg. 2004; 33(8): 804-5.
- Aguilo L, Cibrian R, Bagan JV, Gandia JL. Eruption cysts: Retrospective clinical study of 36 cases. ASDC J Dent Child. 1998; 65(2): 102-6.
- Bodner L, Goldstein J, Sarnat H. Eruption cysts: A clinical report of 24 new cases. J Clin Pediatr Dent. 2004; 28(2): 183-6.
- Alvarez MP, Crespi PV, Shanske AL. Natal molars in Pfeiffer syndrome type 3: A case report. J Clin Pediatr Dent. 1993; 18(1): 21-4.
- Kates GA, Needleman HL, Holmes LB. Natal and neonatal teeth: A clinical study. J Am Dent Assoc. 1984; 109(3): 441-3.
- Buchanan S, Jenkins CR. Riga-Fedes syndrome: Natal or neonatal teeth associated with tongue ulceration. Case report. Aust Dent J. 1997; 42(4): 225-7.
- Massler M, Savara BS. Natal and neonatal teeth: A review of 24 cases reported in the literature. J Pediatr. 1950; 36(3): 349-59.
- Macknin ML, Piedmonte M, Jacobs J, Skibinski C. Symptoms associated with infant teething: A prospective study. Pediatrics. 2000; 105(4 Pt 1): 747-52.
- Swann IL. Teething complications, a persisting misconception. Postgrad Med J. 1979; 55(639): 24-5.
- Wake M, Hesketh K. Teething symptoms: Cross sectional survey of five groups of child health professionals. BMJ. 2002; 325(7368): 814.
- Wake M, Hesketh K, Allen M. Parent beliefs about infant teething: A survey of Australian parents. J Paediatr Child Health. 1999; 35(5): 446-9.
- Wake M, Hesketh K, Lucas J. Teething and tooth eruption in infants: A cohort study. Pediatrics. 2000; 106(6): 1374-9.
- Seward MH. Local disturbances attributed to eruption of the human primary dentition. A survey. Br Dent J. 1971; 130(2): 72-7.
- Coreil J, Price L, Barkey N. Recognition and management of teething diarrhea among Florida pediatricians. Clin Pediatr (Phila). 1995; 34(11): 591-8.
- Buckler JMH. A Reference Manual of Growth and Development. 2nd ed. Oxford, England: Blackwell Science; 1997.
- Victorian Government Department of Human Services. The health of young victorians [online]. Melbourne, Australia: Victorian Government Department of Human Services. October 1998 ]cited 26 August 2009]. Available from URL: http://www.health.vic.gov.au/ healthstatus/ downloads/ hyv.pdf
- Tasanen A. General and local effects of the eruption of deciduous teeth. Ann Paediatr Fenn. 1968; 14(suppl 29): 1-40.
- McIntyre GT, McIntyre GM. Teething troubles? Br Dent J. 2002; 192(5): 251-5.
- Zamani A. Facts Seets for Families. American Academy of Pediatric Dentistry: California Childcare Health Program; 2005.
- Seward MH. The treatment of teething in infants. A review. Br Dent J. 1972; 132(1): 33-6.
- Therapeutic guidelines: Oral and Dental. 1st ed. North Melbourne: Therapeutic Guidelines Limited; 2007.
- Dental Practitioners’ Formulary 2000-2002. London: British Dental Association; 2002.
- Steward M. Infant care. Teething troubles. Community Outlook. 1988; 27-8.
- Jones M. Teething in children and the alleviation of symptoms. J Fam Health Care. 2002; 12(1): 12-3.
All content and media on the HealthEngine Blog is created and published online for informational purposes only. It is not intended to be a substitute for professional medical advice and should not be relied on as health or personal advice. Always seek the guidance of your doctor or other qualified health professional with any questions you may have regarding your health or a medical condition. Never disregard the advice of a medical professional, or delay in seeking it because of something you have read on this Website. If you think you may have a medical emergency, call your doctor, go to the nearest hospital emergency department, or call the emergency services immediately.

 The time when a baby’s first few teeth begin to erupt is called teething.
The time when a baby’s first few teeth begin to erupt is called teething.





